 The latest issue of CASE is now available with intriguing reports, including “Patent Foramen Ovale With Asymmetric Pulmonary Venous Flow Reversal.”
The latest issue of CASE is now available with intriguing reports, including “Patent Foramen Ovale With Asymmetric Pulmonary Venous Flow Reversal.”
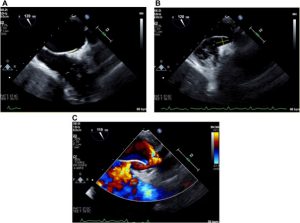
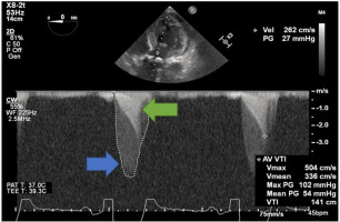
CASE Editor-in-Chief Vincent Sorrell, MD, FASE, remarked, “Every issue of CASE offers readers an opportunity to discover novel insights into commonly seen echo-truths that in fact, turn out to be less specific than initially thought. Take for example the report from Wright et al., which discusses their finding of reversal of the systolic pulmonary vein flow seen with pulsed wave Doppler. The patient did not have mitral regurgitation as the mechanism for this finding, but instead, had an intermittently significant shunt across a PFO. The authors describe their Doppler finding, the literature surrounding the underlying proposed mechanisms, and the clinical correlations. Within their descriptions, they include the possibility that significant left to right shunts may cause a similar systolic flow reversal in the pulmonary vein. In their patient, the PFO flow was minimal at baseline but increased dramatically during deep inspiration. This phasic PFO flow was noted to directly coincide with the phasic pulmonary vein systolic reversal, leading to these authors’ conclusion and helping CASE readers build their differential diagnosis of this finding. They suspect that intermittent increases in LA volume and pressure, similar to previous reports with ASD, were driving this Doppler phenomenon. It is exciting to ponder what our amazing Journal readers will see tomorrow that will inform us to be better stewards of echocardiography.”
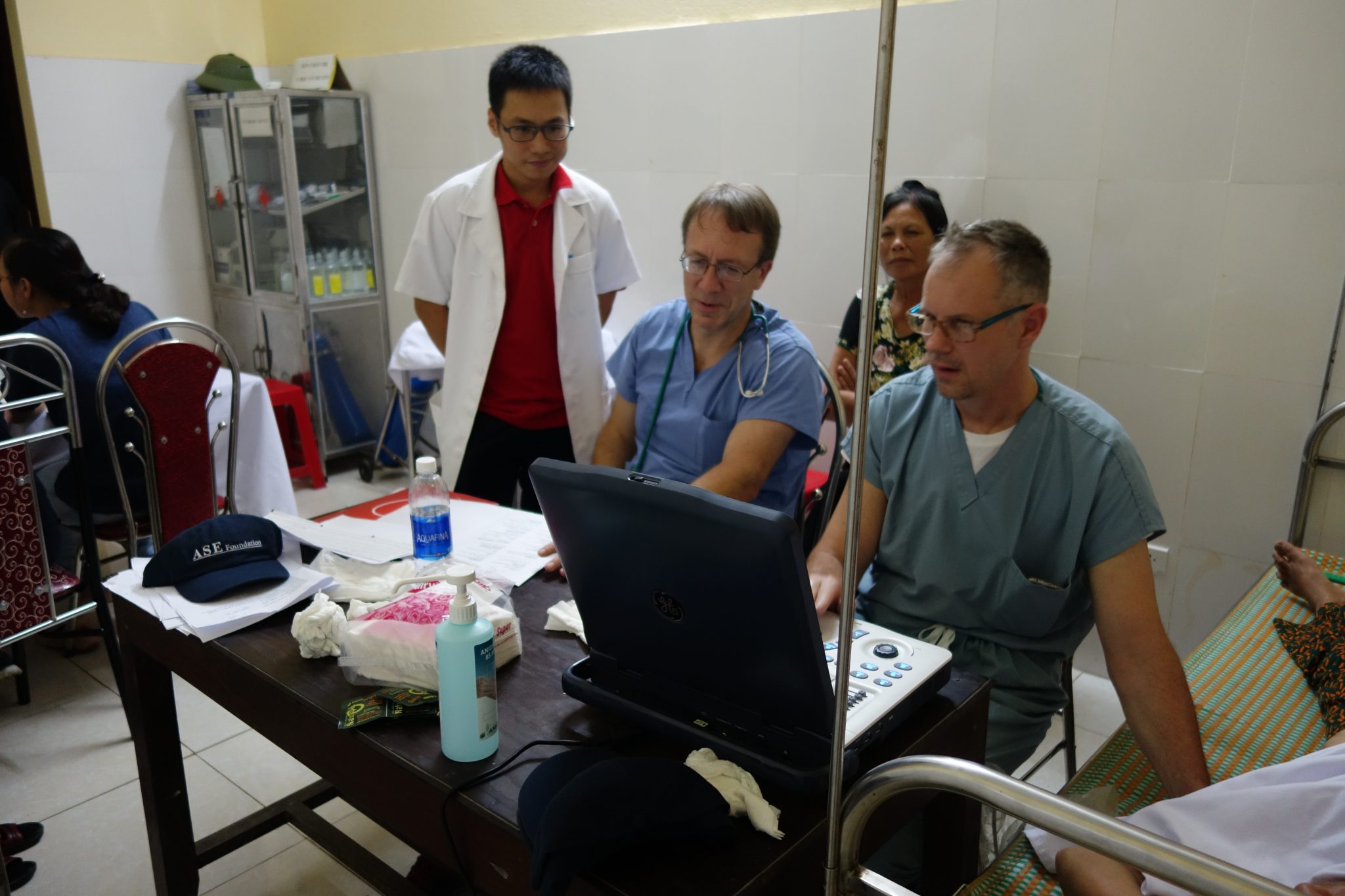
In addition to this Hemodynamic Corner report, this issue features some cases in the Rare But Deadly Findings and Sonographer Spotlight categories. Menon et al. highlight the importance of serial echo in their report on an infant with Kawasaki Disease, whose condition rapidly progresses in wake of early detection and available treatment. Aleem et al. utilize targeted neonatal echo in a critically ill neonate, evaluating cardiac function, ECMO cannulation, and development of a deadly coronary thrombus. Notably, this issue features two reports selected from our recent Sonographer Challenge—a report on caval valve implantation as an innovative approach for treating severe tricuspid regurgitation, and a report of preliminary findings on the use of an agitated saline delivery device in daily clinical practice.
Readers can look forward to Dr. Sorrell’s editorial, which dissects the vital role of contrast in diagnostic imaging. Be sure to check out the latest Unlock the CASE on the CASE homepage, which was the winning entry from the Cardio-oncology SIG Case Competition.
SUBMIT your case report to us! Whether it will be your first time submitting a case or your 50th, we are here to make it a great experience. Email us with questions or submit your report today!



 Effective January 1, 2025, the new CPT code 0932T – Noninvasive detection of heart failure derived from augmentative analysis of an echocardiogram that demonstrated preserved ejection fraction, with interpretation and report by a physician or other qualified health care professional will replace the previous HCPCS outpatient code C9786.
Effective January 1, 2025, the new CPT code 0932T – Noninvasive detection of heart failure derived from augmentative analysis of an echocardiogram that demonstrated preserved ejection fraction, with interpretation and report by a physician or other qualified health care professional will replace the previous HCPCS outpatient code C9786.